Project Update: «Decision-making for Cost-Effective Medical Supply” Preliminary solutions developed and tested in the field
In 2020, the ETH Zurich, EPFL, and ICRC kicked off the EHA program to apply scientific knowledge to improve the performance of humanitarian aid. Our project “Decision-making for Cost-effective Medical Supply” was one of the projects which was set up to benefit from this close collaboration between the Swiss institutions.
At ETH Zurich’s chair of logistics management, Prof. Stephan Wagner’s HumOSCM team is working with the ICRC’s head of Supply Chain Sophie Gligorijevic to assess the delivery of medical supply to health facilities in crisis and conflict regions. In humanitarian response, lives depend upon the timely delivery of goods to often remote and dangerous places. At the same time, a growing funding gap demands that resources like money and capacity are efficiently deployed, so shrinking budgets reach as many beneficiaries as possible.
The fundamental trade-off between cost and service in a supply chain has been well studied and has generated methods and models to optimize the supply chain. The EHA project “Decision-making for Cost-Effective Medical Supply” has been applying this engineering knowledge base to the ICRC medical supply chain, with the intermediate results summarized here.
The project invested over a year of effort to gather data on the material and information flows in a selected medical supply chain, which is considered representative for the organization. The solutions developed for this segment are expected to be adapted and transferrable to other ICRC operations.
The quantitative and qualitative data was then used to map and assess system performance, as well as to identify opportunities for improvement.
In this project, ETH’s HumOSCM lab and ICRC are addressing the following four challenges:
- Reducing Demand Variability and the Bullwhip Effect (completed)
- Bottlenecks in the Geneva Logistics Centre (field-testing)
- Cost of Medical Supply (in progress)
- Improvement of Planning Processes and ERP Adoption (in progress)
1. Reducing Demand Variability and the Bullwhip Effect (concluded)
The project was originally proposed by an ICRC medical logistics specialist who suggested that the ordering patterns at health facilities be measured and controlled. The initial hypothesis was that these orders from the field were highly volatile, and triggered costly cycles of overstock and stockout which propagated upstream to the supplying logistics centres (Nairobi and Geneva in particular).
The review of several years of demand across multiple health facilities did not confirm this hypothesis. The order variability did not result in a measurable bullwhip effect.
In particular, the cost of variability measured in the system did not justify the purchase of an IT system which would limit order quantities (Imprest).
At an operational level, the ICRC logistics team did not consider influence over ordering behavior in the health facilities to be a realistic option. As a consequence, the project therefore shifted its focus to optimizing supply, whose analyses are ongoing and described in section 3 (Cost of Medical Supply).
2. Bottlenecks in Geneva Logistics Centre (Field-testing)
The Geneva Logistics Centre is the main warehouse of the ICRC’s global network for medical and other supplies. Due to its location in Switzerland, it is also the most expensive operation, which deters investments in expansion. Over time, the capacity of the facility has not grown in step with the increasing volume of material which it must handle. Backlogs of shipments had become a chronic issue, with little prospect of improvement since an increase in the workforce in Switzerland is not a viable option.
To diagnose the performance gaps, the joint ETH-ICRC team conducted an in-depth data and system analysis, looking at everything from information flows to parameterization. This work revealed three root causes of shipping delays of requested medical items:
- Standardized configuration of variable supplier lead times
- Suboptimal workload distribution among logistics sites
- Unintended consequences of order frequency policies
In the first case, supplier lead times were configured as a one-size-fits-all standard across the entire medical supply list. This would schedule the delivery of a stockpiled item like paracetomol (which is usually on-hand and ready to ship), exactly like an X-Ray machine, which must be processed as a special order from the manufacturer with long lead times. Although standardization can make sense in other contexts, the consequence of this undifferentiated parameter was the delay of orders. Their delivery dates were always scheduled to accommodate the longest common lead time, whether or not the requested items were on the shelf and available immediately. This left health facilities waiting unnecessarily and possibly motivating them to over-order, which further distorted the demand patterns received by planning teams.
The second and third issues became apparent around the shipment backlog in Geneva. As order volumes increased continuously over time, staff and other capacities remained unchanged. Bottlenecks and pile-ups on the loading docks were the consequence.
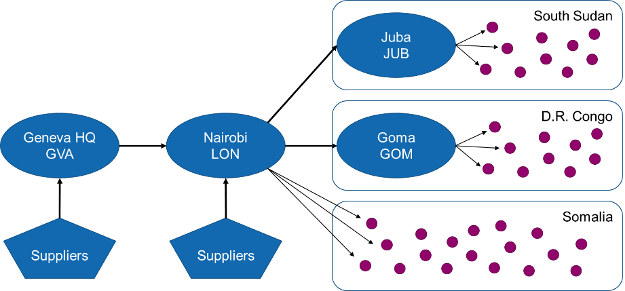
The solution would require that ICRC make the most of existing resources (like facilities and staff and inventory), while minimizing additional investments. After a detailed analysis of both inbound and outbound material flows, the project recommended that the purchasing and inventories of a portion of the 174 standard medical items no longer be managed in Geneva, but shifted to the distribution centre in Nairobi. This reconfiguration of the management functions would not only relieve the bottlenecks in Geneva, but boost the specialization of the regional distribution centre in Kenya. The higher capacity in Nairobi, which already supplies around 210 items to global recipients, could accommodate the additional workload.
The project then turned its attention to business rules. A mathematical model of order fulfilment further revealed that a change in order frequency from once a month, to every two months is further expected to reduce the backlog at the loading dock in Geneva.
Both solutions are currently being tested in preparation of a wider rollout within the ICRC logistics network.
3. Cost of Medical Supply (in progress)
One of the fundamental trade-offs which must be managed in any supply chain is the cost of providing service to those who place orders. The cost of keeping stock in case of demand must be balanced against the cost of stocking out, which in the case of medical supply in war zones, can result in both suffering and mortality.
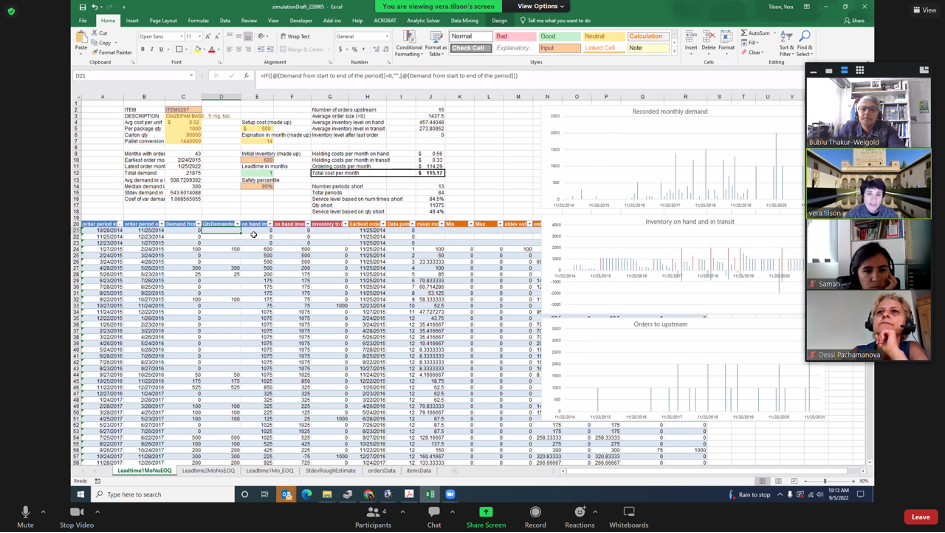
Using real data from their order management systems, and under the guidance of the ETH research team, the ICRC planning team is modeling the trade-off between cost and service in the form of an “efficient frontier”. This simulation is expected to enable “what-if” analyses and support decisions on where to modify or shift investments in inventory.
4. Improvement of Planning Processes and ERP Adoption (in progress)
The steady growth of its operations, and the need to make budgets go further were motivations for the implementation of an organization-spanning ERP system, which supports planning processes. Over time, the new ERP system was rolled out starting at ICRC’s headquarters, then moving to the regions, starting with the large delegations. Among the processes it supports were those which plan supply and demand, which can be challenging. Especially at the field level, these processes required continuous collaboration between disparate teams in logistics, finance, management, and the various programs in the delegation. At the same time, a widespread adoption will be crucial since accurate planning on all levels is the prerequisite for smoother and more efficient medical supply.
As the project studied these processes, it identified degrees of variation in both adoption and compliance. Even while the organization pushed for more acceptance of the new system, actual adoption in certain delegations and in certain programs remains incomplete. The project thus studies the characteristics of both successful system adoptions and the cases where more resistance is observed. Its results will support the ICRC to establish both the IT system and the planning processes as an institutional standard. On the academic side, a deeper understanding of long-term organizational change in non-profit organizations like ICRC contributes to organizational theory, from which other non-profits can learn.
